Traci Hurley says watching her husband battle cancer in late 2021 was harrowing. “It was heartbreaking, and it was awful,” she said. “I lived in fear every day.”
A battle made worse, she says, because so many of the skirmishes were with their insurance company. “No family should have to go through having to fight to get treatment recommended by their physician covered, while fighting for their lives,” she said.
Millions of Americans say they are struggling to get medical care: either unable to pay sky-high deductibles, or, like Dan Hurley, denied coverage for tests and treatment by health insurance companies. Not only were both the Hurleys doctors; Dan, an ear, nose and throat surgeon, was also skilled in cutting through insurance red tape for his patients.
“And yet, we still ran into issues a lot,” Traci said. “If we, as two physicians, had to struggle the amount that we had to struggle to get care approved, what about people who do not have medical knowledge? What’s happening to them every day?”
Dan was an avid hiker, until a nagging backache turned out to be cancer. He was diagnosed with chondrosarcoma, an ultra-rare bone tumor. To try to save his life, the tumor, along with Dan’s hip, had to be removed. Insurance only covered a portion of the costs.
Traci said, “Many of his treatments were denied. We had PET scans, we had CT scans denied. We had chemotherapy, we had radiation, we had certain medications that required prior-authorization, and were denied.”
The basis for the insurers’ denials, Traci said, was that they were “not medically indicated.”
“Make their lives as difficult as possible”
Ron Howrigon, now a consultant, spent two decades working for health insurance companies. “Health insurance companies know that five percent of their members account for 50 percent of all the costs,” he said. “So, I have this huge financial incentive to make their lives as difficult as possible.”
Howrigon says the business model is unlike other industries: “The more your customers use your product, the less money you make. Your incentive is to keep them from using your product.”
How often do insurance companies refuse to cover the cost of medical treatments? It’s hard to tell; health insurance companies are only required to report denial data for plans purchased through healthcare.gov.
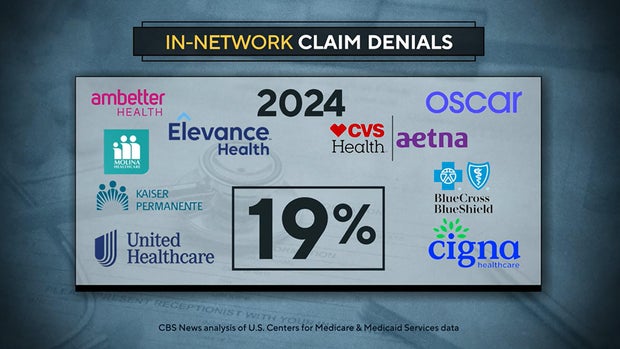
A CBS News analysis of about 1.3 billion federal health insurance claims across three years shows that, in 2024, insurers denied 19% of in-network claims – about 1 in 5.
CBS News
But for the biggest insurer, United Healthcare, that was a steep drop from the preceding two years, when it denied as many as one-third of its federal claims.
While it did not provide data to support it, United Healthcare says that, across all its plans, their initial denial rate is 10%. They also point out that when employers are self-insured, the plans they choose for their employees dictate coverage decisions.
“About 165 million Americans are enrolled in employer-sponsored health care plans, and 65% of them are enrolled in what’s called a self-insured plan,” United said in their statement. “The health insurance company they select provides administrative services such as handling calls from members and paying claims. But as the phrase ‘self-insured’ suggests, it’s the employer’s funds that cover claims payments. …
“Self-insured employers can design their health plans and determine what will and won’t be covered for their employees,” United continued. “It’s important to remember that your health insurer probably isn’t the one that designed it that way. Your employer did.”
“Insurance is out of control”
Dr. Elisabeth Potter, a surgeon who sees as many as 60 patients with breast cancer each week at her RedBud surgery center in Austin, Texas, said, “The insurance companies have, honestly, made it more difficult to be healthy in the United States.”
She says insurance denials actually add to costs: “I have two employees who spend almost all day navigating insurance. It seems that everywhere we turn, there’s an issue, whether it’s an insurance company saying, ‘You know, we won’t cover your surgery at that surgery center,’ or ‘We won’t pay for that medication, we want you to be on a different medication.'”
CBS News
Case in point: On an early morning this past Fall, Jeannie Lee, a 40-year-old mother with breast cancer, was being prepped for a procedure – a lymphovenous bypass – that could have been done two weeks earlier during her double mastectomy, but both her and her husband’s insurance companies refused to cover the cost.
Lee is at high risk for developing a condition known as lymphedema where, Potter said, “It becomes very difficult to just use your arm. It can be painful. It’s swollen. It’s also deforming.”
Lee said, “I’m 40 years old. I have three young kids. It’s very necessary to do this procedure.”
Once Lee was able to obtain financial assistance through a new non-profit set up by Dr. Potter, she was back in surgery. “This patient is having an extra surgery, a separate general anesthetic, because her insurance company wouldn’t cover the surgery,” Potter said. “We could have done this very easily at the same time [as her mastectomy ].”
When she isn’t in surgery, Potter is often on the phone defending her treatment decisions to insurance company medical directors who, she says, often know little about her area of medicine. “Sometimes I get, you know, an ophthalmologist, an eye doctor. It was just completely absurd,” she said.
She sometimes posts her side of those conversations online.
Potter: “So, we’re speaking about lymphedema of the arm. So, this is not an area that you’re familiar with, correct?”
But a video she posted in early January 2025, she says, ended up putting her entire medical practice at risk. While she was in the operating room, Potter says she got a call from United Healthcare. That “urgent” call, she says, was to question why her patient needed an overnight stay in the hospital.
“It’s never happened before. I didn’t know what was going on, but they said it was urgent and I needed to call, and so I did,” she said. “I am operating. I’m doing the right thing for the patient. I’m going to keep her overnight. I walked out of the hospital and I just filmed myself in my unfiltered, you know, moment.”
Potter: “It’s out of control. Insurance is out of control.”
Shortly after she posted that video, she got a letter from the insurance company threatening to sue her for defamation. “I’m taking great care of patients. They’re just trying to scare me into being quiet,” Potter told us.
I asked, “And weren’t you scared?”
“I was scared,” she replied.
United Healthcare has not taken Dr. Potter to court. They declined an on-camera interview, but a company spokesperson says the call was due to an erroneous order, and a doctor would never be asked to leave surgery for a call about an insurance matter.
“It was such a gut punch”
Miranda Yaver, an assistant professor at the University of Pittsburgh, says insurance companies know that only a small percentage of people will actually appeal claim denials.
“All of us are vulnerable to being denied,” she said. “Not all of us can weather the storms easily when it comes to appealing and overcoming these barriers.”
Yaver calls it “rationing by inconvenience.”
“A lot of people don’t know that they even can appeal,” Yaver said.
I asked, “You’re saying that it’s not really the denial that ends up keeping people from getting care, it’s that people give up? “
“Fewer than one percent of those in-network claim denials result in appeal, even though people were winning roughly half the time,” Yaver said.
Clearly, it does pay to appeal, but some patients, like Dr. Dan Hurley, fighting an aggressive cancer, run out of time. Much of his last months were spent, says his wife Traci, on the phone with insurance company personnel: “He would go line by line with them and they’d say, ‘Okay, yeah, we need to get a supervisor involved. We’ll call you back.’ And then they don’t.”
Dan’s goal, she says, was to see insurance companies held to a standard similar to doctors, making them liable for malpractice when they deny lifesaving care. “The act of signing that denial is practicing medicine,” Traci said, “the same way, if a patient came to me and I made a decision about treatment and that decision went sideways, I’m liable. That’s how it works.”
Dan Hurley died on August 3, 2023. One week later, his wife got a letter from the insurance company asking her to pay $80,000 for a round of chemotherapy that had been pre-authorized, but was suddenly retroactively denied. “It was such a gut punch to get it that day,” she said. “This is unbelievable, right? Almost laughable.”
Dan Hurley’s battle has become his widow’s. “There’s a part of me that says, ‘Oh, he would be so proud of me,’ but there’s also part of me that he’d be like, ‘Come on, chop, chop, you got this, let’s go, pick it up, don’t be sad, you know, keep going.’ Because that’s what he was like.”
For more info:
Story produced by Sari Aviv. Editor: Jason Schmidt.